What is a Posterior Pelvic Tilt?
 |
| posterior pelvic tilt |
A posterior rotation of the innominates is indicative of a posterior pelvic tilt. As a result, the person will typically appear to have a relatively flat back and "tucked under" buttocks. Even while the posterior tilt is less frequent than the anterior tilt, it still has many negative effects.
Because of the limited flexibility at the sacroiliac joints, the sacrum and lumbar spine move together with the pelvis when it moves. The vertebrae will stack more vertically on top of one another as a result of the posterior rotation, which will also lessen the lumbar lordosis. Reduction of compressive stresses in the spine and adequate shock absorption are two of the main purposes of lumbar lordosis.
Therefore, the spine's overall capacity to absorb shock is diminished when lumbar lordosis is lost. The intervertebral discs will experience greater compression stresses due to the vertebral bodies' more vertical placement on top of one another. Lumbar disc disease may be influenced by the intervertebral discs' increased degree of compression.
There are a number of causes of posterior pelvic rotations, but the majority result from long-term overuse of one's posture, such as slouching while sitting. If inadequate body mechanics, such as slouching, are repeatedly reinforced, it could worsen posterior pelvic rotation. Therefore, training good body mechanics and postural re-education are necessary in addition to short-term Physical therapies.
Causes of Posterior Pelvic Tilt
The posterior pelvic tilt may be caused by a number of muscle imbalance related causes. The pelvis may rotate posteriorly due to stiffness in the hamstrings and/or abdominal muscles. But because the hamstrings and abdominals are also phasic muscles, as they get tired, they lean toward weakening rather than hypertonicity.
Thus, this postural distortion cannot be caused by hamstring or abdominal tightness alone; rather, it requires a considerable degree of both. More often than not, posterior rotation is an adaptive habit continued by bad sitting and standing Body mechanics.
Posterior Pelvic Tilt Symptoms
Your lower back is under a lot of strain when you have a posterior pelvic tilt. Sciatica, or pain running down the back of one's thigh or glute, is one type of pain that might eventually result from this.
- Weak and tight leg muscles
- Shortened tendons around the pelvic bones
- Feeling of tightness in abdominal muscles
- Hamstring tightness
- Improper balance
- Poor posture
- Reduced Lumbar Lordosis
- Lower Back pain with or without Radiating pain in lower limb
- Sciatica Pain
- Hip Pain with or without Knee pain
A posterior pelvic tilt can be present by any of these variables. This is the moment when your upper body rounds back and your glutes tuck inward.
Long term Side Effects of Posterior Pelvic Tilt
Your entire posture is impacted because your neck and upper back are forced forward in an attempt to correct the improper pelvic position.
A forward head position and a more rounded shoulder, often known as thoracic kyphosis, are common symptoms of posterior pelvic tilt.
The compression strain on the mid and lower back will gradually rise due to posterior tilt. Due to the uneven loading of the spine caused by this increased compression stress, problems such as disk prolapse or disk herniation may result.
In addition, the lumbar curve's rounding places undue strain on your spine and raises the risk of hip, back, and leg pain.
Treatment of the Posterior Pelvic Tilt
The hamstring and abdominal muscle groups should be treated while treating posterior pelvic rotations. They require to get their tightness and myofascial trigger point presence looked upon. On the rectus abdominis muscle, longitudinal stripping and sweeping cross-fiber techniques can be used. It is possible to address the hamstring muscles' role in posterior pelvic tilting.
Treatment for the posterior pelvic tilt must include postural re-education, as was previously described. If soft tissue manipulation is tried without any kind of reinforced and corrected movement patterns, the practitioner is likely to have little success.
Stretches to Fix Pelvic Posterior Tilt:
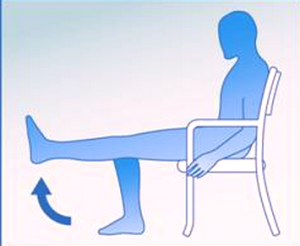
Stretching Your Hamstrings While Seated
Long periods of sitting and standing can cause hamstring tightness, which can result in bad postures such a posterior pelvic tilt. Your hamstring will lengthen as a result of stretching, which will help your body maintain a more neutral pelvic position.
How to do it:
Sit down on a firm chair at first - Extend your left leg in front of you
Aim for three repetitions on each side. Bend forward and reach for your toes until you feel a minor stretch.
Hold nearby for 10 to 20 seconds. Slowly return to the starting position. Repeat on your right side.
Take caution: If you extend the stretch too far, you risk pulling a muscle in your back. Take care not to go overboard. Try transferring this exercise on the floor if sitting in a chair is too challenging for you.
Bhujangasana: Abdominal Press Up (Cobra Pose)
Your tightened abdominal muscles will extend and become more flexible with the help of this stretch, which will enable a more neutral pelvic position.
How to carry it out:
- Start by lying on the floor with your hands flat at shoulder level. - Gradually push your hands up to lift your shoulder off the floor until you feel a slight stretch.
Exhale as you push deeper into the lumbar extension to increase your range of motion.
Try to complete five repetitions.
Piriformis Stretch
The piriformis muscle may tighten up after extended periods of sitting. Stretching this muscle will enable the hip to move normally, which aids in achieving a neutral pelvic position.
How to do it:
Start by lying on your back with your feet flat on the ground and your knees bent.
To begin, place your right ankle over your left knee. Then, grab your left knee and draw it in towards your chest for a few seconds, until your right gluteal muscles stretch. Repeat on the other side. Try to complete three repetitions on each side.
Exercises to strengthen Muscles of the posterior pelvic tilt
Lunges:
Lunges improve quadriceps strength. It may be possible to correct a posterior pelvic tilt by strengthening these muscles.
How to carry it out:
- Start by placing your feet together. Stretch out your left leg in front of you. When your left leg is bowed to a 90-degree angle, your right knee should come into contact with the floor. Resuming your initial position requires pushing up with your left leg. On your right side, repeat. Try to complete three sets of ten lunges on each side.
* When in the lunge position, make sure your knee does not go over your toe as this puts more strain on the knee.
Superman:
Superman assists with correcting improper pelvic alignment by strengthening your lower back and glutes, which are connected to your pelvis.
The exercise can be performed as follows:
Lay on your stomach on the floor with your arms extended in front of you
Slowly raise your chest off the ground and attempt to hold this posture for 30 seconds
Slowly return your body to the beginning position
Try to complete three repetitions.
Leg Lifts
Leg raises assist in strengthening your hip flexors, which become incredibly weak due to the pelvic posterior tilt.
How to carry it out:
- In Supine Position on the soft mat with your legs extended. Keeping your arms straight by your sides, slowly raise your legs off the ground by contracting your abdominal muscles.
– Return your legs to the beginning position slowly.
The secret to this exercise is to solely move your legs; this will help your core muscles grow.
This is a challenging workout; if you have trouble lifting your legs, consider bending your knees a little.
Adjustments to Sleeping
To help you sleep with appropriate posture:
- Stay away of sleeping on your stomach.
- Place a little pillow below your knees if you prefer to sleep on your back.
- A pillow should be placed between your knees if you are a side sleeper.
- Put a tiny pillow or rolled towel beneath your back's arch if you sleep on your back.
- Verify that the cushion and mattress suit the natural curve of your spine.
- You are sat in a posture-supporting chair.
- Your choice of workstation or table should enable you to sit upright and prevent slouching.
- You can either utilise an integrated lumbar support chair or use a pillow for this type of assistance.
- You make the effort to move around and stretch, especially if you spend a lot of time seated.
- Soreness in the lower back.
- Rotation inward at the hip and knee.
- Knee ache and hip pain.
- Hip flexor tension is the cause of sciatica.