What is a Trapezius Muscle Pain?
Trapezius muscle pain can range from mild discomfort to severe, debilitating pain, affecting daily activities and overall quality of life.
One of the main muscles of the back and neck is the trapezius muscle, so named because of its trapezoidal shape. It reaches across the shoulder blades and descends from the base of the skull to the thoracic spine. This large muscle is important for many movements of the upper back, shoulders, and neck, such as pulling, lifting, and rotating the shoulders.
Despite the trapezius muscle's strength and durability, it can become painful or uncomfortable for a variety of reasons, including bad posture, overuse, stress, or injury.
It is essential to understand the causes, signs, and effective treatments of trapezius muscle pain in order to manage this common condition while improving musculoskeletal health. This article discusses the trapezius muscle's anatomy and function, common causes of pain in the area, warning signs, and preventative and therapeutic measures.
Related Anatomy
 |
| Trapezius Muscle Anatomy |
The trapezius muscle is a large, superficial muscle that covers much of the upper back and neck. It is divided into three distinct regions: the upper (or superior), middle, and lower (or inferior) trapezius.
Upper Trapezius:
Origin: Occipital bone (base of the skull) and the spinous processes of the cervical vertebrae (C1-C4).
Insertion: Clavicle (collarbone) and acromion process of the scapula (shoulder blade).
Function: Elevates and upwardly rotates the scapula. It also assists in neck extension and lateral flexion.
Middle Trapezius:
Origin: Spinous processes of the thoracic vertebrae (T1-T5).
Insertion: Medial aspect of the acromion process and superior lip of the spine of the scapula.
Function: Retracts (adducts) the scapula, pulling it toward the spine.
Lower Trapezius:
Origin: Spinous processes of the thoracic vertebrae (T6-T12).
Insertion: Medial end of the spine of the scapula.
Function: Depresses (pulls downward) and upwardly rotates the scapula. It also assists in scapular retraction.
Nerve Supply:
The trapezius muscle is innervated by the spinal accessory nerve (cranial nerve XI) and branches of the cervical spinal nerves (C3-C4).
Blood Supply:
Blood is supplied to the trapezius muscle primarily by branches of the superficial cervical artery, transverse cervical artery, and dorsal scapular artery.
To understand the function of the trapezius muscle and the possible causes of pain and dysfunction, one must have a thorough understanding of its complex anatomy. Any area of the trapezius muscle that is dysfunctional can cause pain, restricted movement, and poor posture. For this reason, it is critical to properly assess the situation and implement targeted interventions to address problems related to the trapezius muscle.
Trapezius Muscle Pain Causes
Causes of Trapezius Pain are:
Poor Posture:
Extended periods of sitting or standing with bad posture can cause the trapezius muscle to become overworked and strained. Muscle soreness and discomfort can arise from the trapezius becoming overstretched and fatigued from slouching or hunching the shoulders forward.
Muscle Overuse
Overuse of the trapezius muscle can result from repetitive motions or activities involving the arms, shoulders, and neck. This usually happens in jobs or activities where lifting, carrying, or reaching overhead for extended periods of time is required.
Muscle Tension and Stress
People may unintentionally tense their necks and shoulders in response to emotional stress, anxiety, or tension, which can increase the tension in the trapezius muscle. Trigger points and muscle soreness can arise as a result of persistent muscle tension.
Trauma or Injury
Acute pain and inflammation can be brought on by direct trauma to the trapezius muscle, such as a fall or impact, which can result in muscle strains, tears, or contusions. Furthermore, over time, repetitive microtrauma from manual labor or sports-related activities can result in chronic muscle injuries.
Neck and Shoulder Strain
Strains to the muscles, ligaments, or joints of the neck and shoulders can cause pain that refers to the trapezius muscle. Secondary trapezius muscle pain can be caused by diseases like cervical spondylosis, whiplash injuries, or shoulder impingement syndrome.
Poor Ergonomics
Pain in the trapezius muscle can be caused by a poorly designed piece of equipment, incorrect lifting techniques, or an incorrectly set up workstation. It's crucial to maintain good ergonomics to avoid tense and sore muscles when performing daily tasks.
Nerve Compression
Referred pain, tingling, or numbness in the muscle can be caused by compression or irritation of the spinal accessory nerve or cervical spinal nerves, which supply the trapezius muscle.
Postural Imbalances
Unbalances in the muscles that surround the trapezius, like those in the pectoral or rhomboids, can cause compensatory movements and put more strain on the trapezius, making it more vulnerable to pain and dysfunction.
Symptoms of Trapezius Muscle Pain
Other Associated Symptoms are:
Shoulder and Neck Discomfort
Trapezius muscle pain frequently manifests as neck, shoulder, and upper back pain. The pain can be dull, achy, or sharp, and its severity ranges from mild to severe.
Muscle Tenderness
When the trapezius muscle is palpated, certain trigger points or the muscle fibers themselves may be tender or tense in certain places.
Restricted Range of Motion
Pain in the trapezius muscles can restrict shoulder and cervical range of motion, making it challenging to execute actions like raising arms overhead, turning the head, or twisting the neck.
Muscle Stiffness and Tightness
Muscle stiffness and tightness are common symptoms of trapezius muscle pain, especially in the upper back and neck. Feelings of discomfort and decreased flexibility may result from this.
Headaches
Tension headaches or cervicogenic headaches can result from pain that radiates from the trapezius muscle to the head and temples. The dull, band-like sensation that surrounds the head is a common symptom of these headaches.
Shoulder Blade Pain
Pain may be localized to the area between the shoulder blades (scapulae), particularly when the middle and lower trapezius muscles are involved.
Trapezius Muscle Spasms
In rare cases, involuntary muscle contractions or spasms may accompany pain in the trapezius muscle, making movement more difficult and uncomfortable.
Numbness or Tingling
Numbness, tingling, or pins and needles may be experienced in the affected area due to compression or irritation of the nerves innervating the trapezius muscle.
Postural Changes
People who experience chronic pain in the trapezius muscle may adopt compensatory postures or movements to ease their discomfort. As a result, there may be more musculoskeletal imbalances and pain throughout time.
Fatigue and Weakness
It may be difficult to carry out daily tasks involving the shoulders and neck when dealing with chronic pain in the trapezius muscle.
Differential Diagnosis
When making a differential diagnosis for pain in the trapezius muscle, other medical conditions that may have similar symptoms are taken into account. Among the possible differential diagnoses are the following:
- Cervical Radiculopathy: Pain, numbness, or tingling that radiates from the cervical spine and may resemble pain in the trapezius muscle is caused by compression or irritation of the spinal nerves. Cervical radiculopathy can cause weakness or changes in sensation in the upper extremities, and it is frequently accompanied by neck pain.
- Rotator Cuff Injury: Damage to the rotator cuff's muscles and tendons in the shoulder can result in pain and a restricted range of motion that can be felt in the neck and upper back. People who have experienced shoulder trauma or who perform repetitive overhead activities are more likely to sustain rotator cuff injuries.
- Cervical Disc Herniation: Herniation of the intervertebral discs in the cervical spine can compress surrounding nerves, causing pain in the neck, shoulders, and arms. Herniated cervical discs can also result in abnormal reflexes, sensory abnormalities, and muscle weakness.
- Thoracic Outlet Syndrome (TOS): The condition known as Thoracic Outlet Syndrome (TOS) is caused by compression of nerves or blood vessels in the thoracic outlet, which is the area between the collarbone and the first rib. TOS symptoms include arm and shoulder pain, tingling, numbness, and weakness. Certain activities or postures that compress the thoracic outlet can make TOS worse.
- Fibromyalgia: This is a chronic pain syndrome that is marked by body-wide musculoskeletal pain, fatigue, and tender points. Although fibromyalgia can include pain in the trapezius muscle, the illness usually presents with several tender points and systemic symptoms.
- Myofascial Pain Syndrome: Referred pain patterns can be caused by the presence of trigger points, which are small, tender, spastic areas of muscle. Although the symptoms of trigger points in the trapezius muscle can resemble those of trapezius muscle pain, they can be distinguished by manual palpation and trigger point identification.
- Postural Syndromes: Musculoskeletal pain in the upper back, neck, and shoulders can result from long-term poor posture or anatomical abnormalities in the spine or shoulders. Managing postural-related pain requires addressing underlying postural imbalances and ergonomic issues.
- Shoulder Impingement Syndrome: Shoulder pain and dysfunction that may be referred to the trapezius muscle area can be caused by impingement of the rotator cuff tendons or bursa between the humeral head and the acromion process of the scapula.
Diagnosis
A thorough evaluation by a medical professional is usually necessary to diagnose trapezius muscle pain. This evaluation may consist of the following elements:
Medical History: The healthcare professional will start by getting details regarding the patient's symptoms, such as where, when, and how much pain they are experiencing, along with any triggers or mitigating factors. A thorough medical history aids in determining any possible contributing factors or underlying causes.
Physical Examination: To evaluate the flexibility, strength, and range of motion of the shoulders, neck, and upper back, a comprehensive physical examination is performed. To find trigger points, tight spots, or tender spots in the trapezius muscle, the medical professional may palpate the muscle.
Neurological Examination: To assess nerve function, reflexes, and sensory function in the upper limbs, a neurological examination may be carried out. This aids in the evaluation of any indications of nerve irritation or compression that might be causing the symptoms.
Imaging Studies: X-rays, CT (Computed Tomography) scans, and MRIs (Magnetic Resonance Imaging) may occasionally be requested in order to rule out underlying structural abnormalities or injuries in the neck, shoulders, or spine. These imaging modalities can assist in locating any possible sources of pain or dysfunction as well as provide detailed images of the musculoskeletal structures.
Nerve Conduction Studies and Electromyography (EMG): These tests may be suggested to evaluate the electrical activity and function of the muscles and nerves that supply the trapezius muscle. Neurological disorders and abnormalities of the muscles can be diagnosed with the aid of nerve conduction studies and EMG.
A diagnosis of trapezius muscle pain or another musculoskeletal condition may be made in according to the evaluation's results. The recommended course of treatment will be individualized to target the particular underlying cause and reduce symptoms; this may include a mix of complementary therapies, medication, physical therapy, and lifestyle changes.
Treatment of Trapezius Muscle Pain
A combination of conservative treatments targeted at pain reduction, muscle function enhancement, and addressing underlying contributing factors is usually used to treat trapezius muscle pain.
Common treatment options are:
Rest and Activity Modification: Reducing activities that aggravate pain in the trapezius muscle or taking a brief break from them can help manage symptoms and stop the muscle from getting worse. It's crucial to stay out of positions or repetitive movements that put strain on the trapezius muscle during the first stages of treatment.
Physical therapy: A customized program for physical therapy can help improve flexibility, strengthen the trapezius muscle, and address postural imbalances. To lessen discomfort and accelerate healing, practitioners can use manual therapy, stretching exercises, therapeutic exercises, and modalities like TENS, IFC Machine, heat or ice therapy.
Pain management: Nonsteroidal anti-inflammatory medications (NSAIDs) available over-the-counter, such as ibuprofen or naproxen, can help lessen pain and inflammation caused by pain in the trapezius muscle. For temporary pain relief, doctors may occasionally prescribe prescription drugs or muscle relaxants.
Trigger Point Therapy: Tightness and tension in the trapezius muscle can be released with the use of manual techniques like trigger point massage, myofascial release, or dry needling. Localized pain relief and improved muscle function can be achieved by focusing on trigger points located within the muscle.
Posture Correction: Preventing recurrent pain in the trapezius muscle requires addressing underlying postural imbalances and ergonomic factors. It might be advised to provide education on good posture for everyday tasks, workplace ergonomics, and ergonomic adjustments.
Stress management: By promoting relaxation and easing muscle tension, stress-reduction methods like yoga, deep breathing exercises, mindfulness meditation, and relaxation exercises can lessen the chance of aggravating trapezius muscle pain.
Therapeutic modalities can be used to relieve pain, lower inflammation, and encourage tissue healing in the trapezius muscle. These include heat therapy, cold therapy, ultrasound, and electrical stimulation.
Lifestyle Changes: Adopting healthful routines like consistent exercise, enough sleep, a balanced diet, and adequate hydration can promote general musculoskeletal health and lower the incidence of pain and dysfunction in the muscles.
Ergonomic Modifications: Changing the way that workstations, chairs, computers are set up, and lifting is done can help lessen the strain that regular activities place on the trapezius muscle and lower the chance of developing muscle soreness.
Injections: For localized pain relief and to reduce inflammation in the trapezius muscle, corticosteroid injections or trigger point injections may be considered in certain situations.
Physiotherapy Treatment of Trapezius Muscle Pain
Physiotherapy is essential for treating pain in the trapezius muscle because it corrects muscle imbalances, restores mobility, increases strength, and encourages good posture.
The following elements of a physiotherapy treatment plan for pain in the trapezius muscle may be available:
Manual Therapy Techniques:
- Soft tissue mobilization: A massage technique used to ease the trapezius muscle's tightness and tension.
- Joint mobilization: Mild manual techniques to ease shoulder and neck stiffness and increase joint mobility.
Therapeutic Exercises:
- Stretching exercises: Focused stretches to increase flexibility and decrease muscle tension in the trapezius muscle.
- Strengthening exercises: Postural muscles are the emphasis of these progressive resistance workouts, which aim to strengthen the trapezius and surrounding muscles and support good alignment and stability.
- Scapular stabilization exercises: These exercises help to prevent shoulder impingement and lessen strain on the trapezius muscle by enhancing scapular control and muscle balance.
Postural Correction:
Instruction on ergonomic adjustments, daily activities, and work tasks that promote good posture to avoid straining the trapezius muscle.
exercises for postural retraining to enhance awareness and alignment of the head, shoulders, and spine.
Modalities:
Applying heat packs or warm compresses to the trapezius muscle to improve blood flow, ease tension, and reduce pain is known as heat therapy.
Cold therapy: Applying ice or cold packs to the trapezius muscle to relieve pain and reduce inflammation.
Electrical stimulation: To reduce pain and encourage muscle relaxation, neuromuscular electrical stimulation (NMES) or transcutaneous electrical nerve stimulation (TENS) may be utilized.
Trigger Point Treatment:
By deactivating trigger points in the trapezius muscle, trigger point release techniques—such as manual pressure, ischemic compression, or dry needling—can lessen referred pain patterns.
Learning and Self-Control:
Patient education regarding ergonomics, good body mechanics, and ways to avoid straining muscles and having trapezius muscle pain recurrence.
guidance on self-care practices, stretching regimens, and at-home workouts to speed up recovery and preserve musculoskeletal health.
Gradual Rehabilitative Intervention:
Progressive increase in activities and exercises as function improves and pain subsides, emphasizing everyday living activities and functional movements.
Monitoring development and modifying the treatment plan in accordance with each patient's needs and preferences.
An comprehensive physiotherapy strategy catered to the requirements and objectives of the patient can successfully treat pain in the trapezius muscle, restore function, and enhance quality of life. To maximize results and achieve long-term musculoskeletal health, the patient and physiotherapist must collaborate and communicate on a regular basis.
Exercises for Trapezius Muscle Pain
The goals of exercises for pain in the trapezius muscle are to reduce stress, enhance muscle strength and flexibility, and encourage good posture.
 |
| Upper Trapezius Stretch |
The following efficient exercises can help reduce pain in the trapezius muscle:
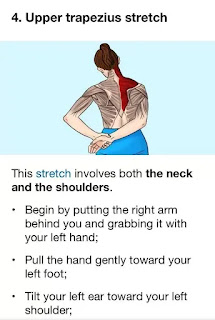
Upper Trapezius Stretch:
- Keep your back straight and sit or stand tall.
- Till you feel a stretch along the side of your neck, gently tilt your head to one side and bring your ear towards your shoulder.
- After holding the stretch for 15 to 30 seconds, move on to the opposite side.
- Two to three repetitions per side.
Levator Scapulae Stretch:
- Take a tall stance or sit upright, then slowly turn your head to the side and look over your shoulder.
- Place your hand on the top of your head and apply gentle pressure to increase the stretch.
- Hold the stretch for 15-30 seconds, then switch to the other side.
- Repeat 2-3 times on each side.
Scapular Retraction:
- Stand with your back against a wall or in a neutral position.
- As though you were attempting to hold a pencil between your shoulder blades, squeeze them together.
- Hold the squeeze for 5-10 seconds, then relax.
- Repeat for 10-15 repetitions.
Shoulder Shrugs:
- Stand or sit with your arms at your sides.
- Shrug your shoulders upwards towards your ears as high as possible.
- Hold for 1-2 seconds, then lower your shoulders back down.
- Repeat for 10-15 repetitions.
Trapezius Strengthening with Resistance Bands:
- A stable object at waist height should be used to fasten one end of a resistance band.
- Hold the other end of the band in one hand and stand with your side facing the anchor point.
- Keep your arm straight and pull the band diagonally across your body, engaging the trapezius muscle.
- Slowly return to the starting position.
- Perform 10-15 repetitions on each side.
Neck Retraction Exercise:
- Maintain a neutral head posture while sitting or standing.
- Gently tuck your chin towards your neck, creating a double chin.
- Hold for a few seconds, then release.
- Repeat for 10-15 repetitions.
Wall Angels:
- Stand with your back against a wall and your arms bent at 90 degrees with your elbows and wrists touching the wall.
- Slowly slide your arms upwards along the wall while keeping your elbows and wrists in contact with the wall.
- Squeeze your shoulder blades together the entire time you perform the movement.
- Return your arms to the starting position by sliding them down.
- Repeat for 10-15 repetitions.
Thoracic Extension Stretch:
- Sit on the floor with a foam roller positioned horizontally under your upper back.
- Support your head with your hands, keeping your elbows bent.
- Slowly lean back over the foam roller, arching your upper back and extending your thoracic spine.
- After holding the stretch for 15 to 30 seconds, go back to your starting posture.
- Repeat 2-3 times.
Regularly perform these exercises, paying attention to your form and deliberate movements. Stretch lightly at first, then progressively increase the resistance and intensity as tolerated. Before beginning any new exercise program, especially if you have pre-existing health conditions or concerns, get advice from a medical professional or physical therapist.
Keeping a healthy lifestyle, practicing proper posture, and putting ergonomic techniques into practice can all help prevent pain in the trapezius muscle.
The following advice can help avoid pain in the trapezius muscle:
Maintain Proper Posture:
Maintain a straight back, relaxed shoulders, and a head that is in line with your spine when you sit or stand.
Stay away from hunching forward or slouching as these postures can strain the trapezius muscle and cause imbalances in the muscles.
Take Regular Breaks:
Take frequent breaks to stand up, stretch, and move around if your job requires you to sit at a desk for extended periods of time or if it's sedentary.
Throughout the day, gently stretch your shoulders and neck to release tension and avoid stiffness.
Practice Ergonomic Work Habits:
To encourage neutral posture and reduce strain on the trapezius muscle, rearrange your workspace.
In order to lessen neck strain, place your computer monitor at eye level and use an ergonomic chair with adequate lumbar support.
Benefit from ergonomic add-ons like supportive cushions, adjustable desks, and ergonomic keyboards.
Use Proper Lifting Techniques:
Use your leg muscles to lift heavy objects instead of your back and shoulders by bending your knees and maintaining a straight back.
When lifting, keep the object close to your body and try not to twist or reach awkwardly.
Stay Active and Exercise Regularly:
Exercise on a regular basis to build strength in the muscles of your neck, shoulders, and upper back, especially the trapezius muscle.
Include activities that help you maintain good posture, like core and back strengthening exercises.
Practice exercises that promote flexibility and mobility, like yoga, Pilates, or swimming.
Manage Stress and Tension:
To release tension in your shoulders and neck, try stress-reduction methods like deep breathing, meditation, or mindfulness.
Throughout the day, take breaks to unwind and reduce stress, particularly if you're dealing with a heavy workload or emotional strain.
Drink plenty of water and eat a balanced diet:
In order to keep muscles hydrated and avoid dehydration, which can exacerbate tension and cramping in the muscles, drink lots of water throughout the day.
To enhance overall muscle health and function, maintain a well-balanced diet high in vitamins, minerals, and nutrients.
Get Adequate Sleep:
Make sure you are getting enough restorative sleep every night by making quality sleep a priority.
Invest in pillows and a supportive mattress to help maintain healthy spinal alignment and lessen shoulder and neck strain when you sleep.
These preventive steps can help lower your chance of experiencing pain in your trapezius muscles and improve your overall musculoskeletal health.
Summary
In summary, pain in the trapezius muscle is a common condition that can greatly affect everyday activities and quality of life. Effective management and prevention of trapezius muscle pain require an understanding of its anatomy, causes, symptoms, and available treatments. The most common causes of pain in the trapezius muscle are injury, stress, poor posture, and overuse of the muscles.
Physiotherapy is essential for reducing pain in the trapezius muscle and enhancing muscle function and mobility. It includes manual therapy techniques, therapeutic exercises, and modalities. Furthermore, preventing trapezius muscle pain can be achieved by putting preventive measures into practice, such as maintaining good posture, adopting ergonomic work habits, being active, controlling stress, and getting enough sleep.
Through the implementation of focused interventions and a comprehensive approach to musculoskeletal health, people can effectively manage pain in the trapezius muscle, enhance their general quality of life, and avoid further episodes of pain. For a customized assessment and treatment recommendations, it's crucial to consult a healthcare provider if you suffer from severe or chronic muscle pain. People may achieve optimal musculoskeletal health and long-term relief through preventive care and lifestyle adjustments.






