|
Trapezius Pain
|
Trapezitis is a condition that involves inflammation of the trapezius muscles, which are located on the back and neck. The trapezius muscles originate from the base of the skull and run all the way down to the middle of the back.
They are responsible for moving, rotating, and stabilizing the scapulae (shoulder blades). The main symptom of trapezitis is pain in these areas, which can be exacerbated by movement.
What is a trapezius?
 |
| What is a trapezius |
This muscle lies at the back of the neck and helps in shrugging movement of the shoulders along with upward movement of the head. Unlike torticollis, the pain and stiffness due to trapezitis, is episodic and lasts for 3-5 days at a time. Bad posture is frequently incriminated as the cause for trapezitis.
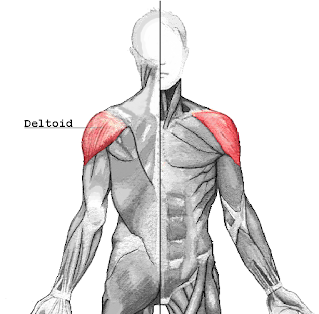
Trapezius muscle is a large muscle on the back of the human body that serves as one of the main muscles of the back, as well as an important muscle for posture and stability. It is divided into three parts: the upper trapezius, middle trapezius, and lower trapezius.
The upper trapezius is located above the shoulder blades and it pulls them up and together. The middle trapezius is located in between the shoulder blades and it draws them down and together. The lower trapezius attaches below the shoulder blades and it pulls them down and together.
Watching television or working on a computer with an awkward posture, or even the use of a thick pillow can cause frequent episodes of neck spasm. The pain of trapezitis can be felt more during extension of the neck backwards as in looking upwards. The trapezius muscle at the back of the neck becomes hard and stiff and a light massage to this area tends to relieve the pain.
It may lead to localized pain,radiating pain towards shoulder and sometimes headache as an indirect consequence.The best way to avoid this pain is taking rest between long working hours and following a relaxation routine of 2-3 minutes after every 45-60 minutes of work.
It allows sideways movements to some extent, which keeps the other neck muscles active and maintains their strength. However, excessive use can weaken the neck muscles (disuse atrophy) and make way for vertebral diseases which are difficult to recover from. Hence, the use of a cervical collar should be only restricted to acutely painful episodes !
Causes:
- Poor postures
- Carrying weight on the upper back put stress on the muscles
- Repeatedly keeping the head still or down during the swing.
- Monotonous jobs with highly repetitive work
- Forceful jerky Activity
- High level of static contractions
Above mentioned any cause or combination of these factors are rsponsible causes of Chronic trapezitis in the working population.
Women more often experience trapezius pain and develop regular pain than men do. This may be due to their jobs. Women’s work tasks involve more static load on the trapezius muscles, high repetitiveness, low control, and high mental demands, which are all risk factors for developing trapezius disorders.
Symptom's of Trapezitis:
- Pain in the upper back and around the neck sometimes radiating pain down to arm, forearm or hands because of Cervical spondylosis.
- Trapezius Muscle Pain with Inflammation
- Trapezius muscle Spasm
- Neck Stiffness / Muscle tightness
Diagnosis
When a healthcare provider diagnoses trapezius muscle inflammation, also known as trapeziitis, they will usually perform a comprehensive medical history review and physical examination. The medical professional may check the affected area for soreness, edema, and limited range of motion during the examination. They might also ask about particular symptoms like stiffness, pain, or trouble moving in a certain way.
Imaging tests, such as MRIs, ultrasounds, or X-rays, may occasionally be prescribed in order to evaluate the extent of any inflammation or injury to the trapezius muscle or to rule out other possible causes of the symptoms.
Giving the healthcare provider as much information as possible about your symptoms, movements or activities that aggravate or relieve the pain, and any recent injuries or events that might have contributed to the condition is crucial.
Treatment of Trapezitis Pain
A combination of conservative treatments targeted at lowering pain, inflammation, and accelerating healing is usually used to treat trapeziitis, or inflammation of the trapezius muscles.
Here are a few typical treatment approaches:
Rest: In order to enable the injured muscles to heal, it is essential that they receive enough rest. Preventing additional irritation can be achieved by avoiding activities that increase pain or strain on the trapezius muscles.
Applying ice packs to the affected area can help reduce inflammation and ease pain. Another option is to use heat therapy. Warm compresses or heating pads, which are forms of heat therapy, can also help to ease muscle tension and increase blood flow.
For Pain Relief: Acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) are over-the-counter pain relievers that can help manage the pain and discomfort caused by trapeziitis. But, it's crucial to take these drugs exactly as prescribed and speak with a doctor if you have any underlying health issues or concerns.
Physical Therapy: To strengthen the trapezius muscles, increase flexibility, and address any postural imbalances that may be causing the condition, a physical therapist can create a customized exercise program. Treatment plans may also include manual therapy techniques like trigger point release, massage, and stretching exercises.
Stress management: Tension in the muscles and trapezius pain can both be made worse by stress. Symptoms may be lessened by practicing stress-reduction methods like yoga, mindfulness meditation, deep breathing exercises, or relaxation techniques.
Avoiding Triggering Activities: Reducing or eliminating movements or activities that exacerbate trapezius pain can help to keep flare-ups at a minimum and aid in the healing process. This might involve altering your workspace, lifting methods, or recreational activities.
Alternative Therapies: Acupuncture, chiropractic adjustments, and herbal supplements are some of the alternative therapies that some people use to treat their trapezius pain.
However, prior to attempting any alternative treatments, it is essential that you speak with a licensed healthcare provider.
Physiotherapy Treatment
The treatment of trapezitis is conservative and consists of analgesics and muscle relaxants during the painful episode of neck spasm. This should be coupled with complete rest to the muscle which is ensured with a soft cervical collar.
Neck muscle strengthening exercises and good posture habits should be followed after complete relief from pain to prevent further episodes of trapezitis.
Sometimes after frequent painful episodes a person develops certain trigger points at the back of the neck which tend to remain painful even after the acute episode. Such trigger points are to be identified correctly and are to be treated with local steroid injections. 2-3 injections seperated by an interval of 15 days generally suffice for cure of trigger points in trapezitis.
The soft cervical collar is an excellent orthosis for pain relief in TRAPEZITIS. It prevents the nodding movements which are known to put stress on the trapezius.
- Reduces pain through advanced modalities (IFT, TENS are Helpful)
- Reduces muscle spasm (Use of Ice Pakc / Hot Pack)
- Reduces tightness. (Trapezius Stretching Exercise)
- Alignment correction through manual therapy. (Mobilization exercise)
- Taping technique
- Reflexology
In case of severe inflammation, Cryotherapy (Ice Pack) and Electrotherapy modalities are help in reducing pain.
How to Prevent Trapezitis Pain?
There are a few things you can do to lessen the chance of strain or injury to the trapezius muscles in order to prevent trapeziitis, or inflammation of the muscles:
- Maintain good posture: When standing, sitting, and moving around, adopt good posture. To reduce shoulder and neck strain, make sure your workstation's ergonomics are optimal and avoid slouching.
- Take regular breaks: If your job involves prolonged sitting or repetitive movements, make sure you take regular breaks to stretch and switch positions. This can lessen the chance of inflammation and help avoid overusing the trapezius muscles.
- Exercises for stretching and strengthening: Make sure your exercise routine includes regular exercises for the neck, shoulders, and upper back. This can lessen the chance of strain and injury by increasing muscle strength and flexibility.
- Use safe lifting techniques: To prevent overstretching your shoulders and back muscles, use safe lifting techniques when moving heavy objects. Keep your back straight, bend at the knees, and lift using your legs instead of your back.
- Control your stress: Stress can lead to tense muscles and raise the possibility of developing inflammation in the trapezius muscle. To ease tension and relax the muscles, try stress-reduction methods like yoga, meditation, or deep breathing.
- Stay hydrated and nourished: Drink lots of water throughout the day to keep your muscles hydrated and at their best for maximum muscle function. Stay nourished and hydrated. Consume a well-balanced diet high in nutrients, minerals, and vitamins to help with muscle repair and health.
- Prevent overexertion: Take it slow when engaging in physical activities and try not to exert too much energy, particularly if you are not used to a particular movement or exercise regimen. Increase the duration and intensity of your workouts gradually to avoid straining your muscles.
- Make ergonomic adjustments: To lessen the strain on your trapezius muscles, if your job involves repetitive or extended use of the arms and shoulders, you should think about making ergonomic adjustments to your workstation or equipment.
You can reduce your risk of developing inflammation in your trapezius muscle and maintain the best possible condition of your muscles by adopting these preventive measures into your everyday routine.
Conclusion
In conclusion, inflammation of the trapezius muscle, or trapeziitis, can result in pain and discomfort in the neck and upper back. Options for treatment include rest, massage, stretching, ice or heat therapy, painkillers, physical therapy, posture correction, and lifestyle modifications.
The risk of developing trapeziitis can be decreased by taking preventive measures like keeping a straight spine and staying away from overexertion. For individualized care, speaking with a medical expert is crucial to efficient management.
Other related Article
 Structure:-
Structure:- Innervation:-
Innervation:- Structure:-
Structure:- Innervation:-
Innervation:-