What is the Subscapularis Muscle?
 |
| Subscapularis Muscle |
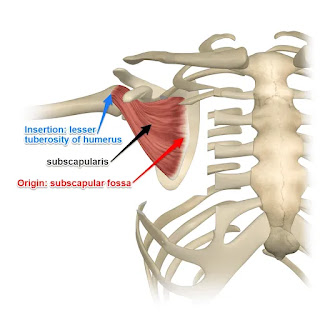
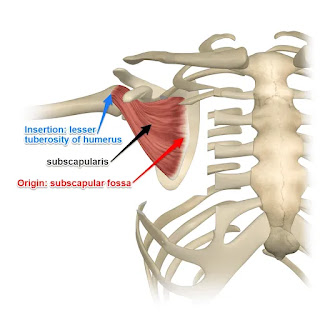
The subscapularis is a broad, triangular muscle that inserts into the front of the shoulder-joint capsule, the lesser tubercle of the humerus, and the subscapular fossa.
It is one of the four rotator cuff muscles, along with the teres minor, infraspinatus, and supraspinatus. The biggest and strongest rotator cuff muscle is the subscapularis.
Weakness in internal rotation results from function loss caused by injury to the muscle or tendon. The preferred course of therapy for tendinopathies and partial tears is non-operative care.
If conservative therapy is unsuccessful, (1) surgical surgery may be necessary; (2) based on the individual’s activity level or occupation (athletes, for example); and (3) in the event of full-thickness rips.
Structure
A thick fascia covering the subscapularis joins to the scapula at the borders of the attachment (origin) of the subscapularis.
The fibers of the muscle merge into an insertion tendon after passing laterally from the muscle’s origin. The glenohumeral (shoulder) joint capsule and the tendon are intermingled.
A bursa sits between the tendon and a bare spot at the lateral angle of the scapula the neck of the scapula. It is connected to the cavity of the shoulder joint by an opening in the joint capsule. The serratus anterior and subscapularis are divided by the subscapularis (supra serratus) bursa.
Origin of Subscapularis muscle
It originates from the bottom two-thirds of the groove on the axillary border (subscapular fossa) of the scapula, the intermuscular septa (which form ridges on the scapula), and the medial two-thirds of the scapula's costal surface.
Aponeurosis, which divides the muscle from the teres major and the long head of the triceps brachii, is the source of some fibers. Tendinous laminae, which cross the muscle and are linked to ridges on the bone, are the source of other fibers.
Insertion of Subscapularis muscle
It attaches to the anterior portion of the shoulder joint capsule as well as the smaller tubercle of the humerus. Tendinous fibers penetrate the bicipital groove and extend to the larger tubercle.
Nerve Supply
The posterior cord of the brachial plexus (C5 to C7) contains branches that give rise to the subscapular nerve, which trifurcates into the upper, middle, and lower subscapular nerves. Both the upper and lower subscapular nerves supply the subscapularis.
The cranial half of the muscle is innervated by the upper subscapular nerve, whereas the caudal half of the muscle is innervated by the lower subscapular nerve, which bifurcates into two branches.
The latissimus dorsi muscle is innervated by the middle scapular nerve, also referred to as the thoracodorsal nerve, whereas the teres major is innervated by the inferior branch of the lower subscapular nerve.
Blood Supply and Lymphatics
The main blood supply to the subscapularis muscle is provided by the subscapular artery, which is a branch of the axillary artery. The lymph nodes in the axilla receive lymph drainage.
Course of the Muscles
The subscapularis muscle enters into the humerus’s lesser tubercle after starting at the subscapular fossa. The muscle adducts the humerus and spins it inside out. In the bicipital groove, the bicep tendon is located beneath the subscapularis tendon.
Innervation
The upper and lower subscapular nerves (C5–C6), which are branches of the posterior chord of the brachial plexus, supply the subscapularis.
Actions/movements
The humerus’s internal rotation is its primary function. In specific postures, it aids with shoulder adduction and extension.
The actions of this muscle are significantly influenced by the position of the arm: when the arm is raised, the subscapularis pulls the humerus forward and downward; when the humerus is fixed, the insertion of the subscapularis can act as an origin and cause the inferior border of the scapula to abduct.
Function of Subscapularis muscle
As the proximal humerus is fixed during elbow, wrist, and hand motions, the subscapularis helps to stabilize the shoulder joint. It is an effective barrier that keeps the humerus’ head from moving forward in front of the shoulder joint.
Surgical Considerations
Partial tears do not require surgery for treatment. When a patient fails conservative care and there is a full-thickness tear, a surgical examination may be necessary, depending on the patient’s activity level and job.
Either an open method or an arthroscopy is used to do surgery. Pathology of the biceps often co-occurs and may need tenotomy or tenodesis.
Clinical significance
The subscapularis etiology of shoulder pain can be caused by tears, tendinopathy, and tendonitis. The most common cause of tendonitis in the subscapularis is overuse from throwing or overhead sports putting the tendon in touch with the coracoid process.
When the symptoms worsen over time and tendon remodeling starts tendinopathy results. Acute rotator cuff tears in athletes who use overhead motion are more common than chronic degenerative injuries from overhead usage.
Subscapularis tears occur less frequently than tears in other rotator cuff tendons. When tears do occur, they are usually caused by a lesser tubercle avulsion, an anterior shoulder dislocation, falling on the outstretched arm during shoulder abduction, or rotator cuff tears.
To Know Shoulder Impingement Click Here
Examination
There is no reliable test for the subscapularis, making isolating its activity from other shoulder joint medial rotators challenging.
The approved clinical test for evaluating the subscapularis is the Gerber Lift-off test. The sensitivity of the bear hug test for subscapularis muscle injuries is great. Significant subscapularis tearing is indicated by positive bear-hug and belly press tests.
Imaging
A gratifying and thorough subscapularis evaluation cannot be obtained with a single imaging tool or method; instead, a combination of the axial MRI / long-axis US and sagittal oblique MRI / short-axis US planes appears to produce meaningful findings.
Furthermore, subscapularis tendon rips have been linked to smaller tuberosity bone alterations. Cyst-related observations appear to be more sensitive when paired with findings related to cortical abnormalities.
Fatty infiltration of the superior sections of the subscapularis muscle, while sparing the inferior regions, is another characteristic that is commonly observed.
It is simple to identify between the supraspinatus and subscapularis tendon because the long biceps tendon disappears from the shoulder joint through the rotator cuff interval. The interval sling is made up of those two tendons.
Ultrasonography
Mack and colleagues devised an ultrasonographic technique that allows for the exploration of nearly the whole rotator cuff in six phases. It makes the whole region visible, from the sub-edge of the subscapularis tendon to the point where the musculus teres minor and the infraspinatus tendon meet.
The subscapularis tendon is the subject of one of the six stages. Initially, the examiner directs the applicator to the proximal humerus in a direction that is as close to the sulcus intertubercularis as feasible. Gliding now to the medial side reveals the subscapularis tendon’s insertion
Longitudinal plane of the musculus subscapularis and its tendon
The subscapularis tendon is 3-5 centimeters below the surface. It is worth attempting to display using a very penetrating 5 MHz linear applicator since it is quite deep for ultrasonography. As it turned out, it made a thorough examination of the muscle that immediately borders the scapula easier.
Nevertheless, the requisite level of mapping is not achieved for the major interest tendon. According to anatomical study, the ventral portion of the joint socket and its labrum can only be seen by external rotation. When the tuberculum minus is in the neutral position, it blocks the vision.
Tissue harmonic imaging
Tissue harmonic imaging, or THI, is increasingly recognized and employed in addition to traditional ultrasonography, primarily in abdominal imaging.
THI uses harmonic frequencies that are not in the incident beam and that come from within the tissue as a result of nonlinear.
Wavefront propagation. Higher contrast resolution may result from these harmonic signals since they may emerge differentially at anatomic locations with comparable impedances.” In comparison to the traditional US, it offers a much lower inter- and intraobserver variability, an elevated signal-to-noise ratio, and greater contrast resolution.
Furthermore, common US artifacts including side-lobe, near-field, and reverberation artifacts may be all but eliminated. As previously indicated, THI has already improved cardiac, vascular, breast, and abdominal sonography.
THI has not been used extensively for musculoskeletal issues, despite the method’s potential benefits. For instance, the still difficult distinction between partial- and full-thickness rotator cuff tears depends on the existence of a hypoechoic defect and/or the loss of the outer tendon convexity/non-visualization of the tendon.
Strobel K. et al. have concluded that using THI can lead to generally better visibility of joint and tendon surfaces, notably superior for subscapularis tendon anomalies, as compared to a standard MR Arthrography.
Pathologies
There are three trigger sites in the subscapularis; the two most prevalent ones are located close to the muscle’s outer border. Fortunately, the inside edge of the muscle trigger point is far less frequent because it is almost tough to manually release and palpate.
Pain referred from subscapularis trigger points is mostly felt in the posterior shoulder area, extending down the back of the upper arm and into the shoulder blade region. There may also be a distinct “band” of transferred pain that surrounds the wrist. The client usually knows that they have wrist discomfort, but they do not believe that it is connected to their shoulder ache.
Throwers often cause injuries to it. Applying pressure to the tendon insertion on the inside of the upper arm will cause discomfort and tenderness. Pain when moving the shoulder, particularly when the arm is elevated above the shoulders, is one indication of subscapularis tendinitis.
You can feel as though you are unable to raise your arm due to an overused subscapularis muscle. It may even be the cause of your frozen shoulder.
Tests For Subscapularis
Lift-Off Test
The lift-off test, often known as “Gerber’s Test,” was first explained by Gerber and Krushell in 1991.
When examining a standing patient, the patient is requested to place their hand behind their back such that the dorsum rests on the area of the mid-lumbar spine. By extending at the shoulder and maintaining or increasing internal rotation of the humerus, the dorsum of the hand is elevated off the back.
A typical lift-off test consists of the ability to actively raise the hand’s dorsum off the back. When the dorsum cannot be moved off the back, the lift-off test is abnormal and suggests a ruptured or dysfunctional subscapularis.
Bear Hug Test
The patient is instructed to do the Bear Hug Test by placing the palm of their afflicted arm on the shoulder of the person opposite them, with their elbow at the maximum anterior translation position in front of their torso.
The doctor places an external rotational force on the patient’s forearm and instructs the patient to hold that posture.
If the patient is unable to hold his arm in place or exhibits weakness in internal rotation as compared to the opposite side, the test is positive and suggests a tear or dysfunction in the subscapularis muscle.
Belly Press Test
The affected arm is positioned on its side, the shoulder flexed to a 90-degree angle, and the palm rests on the patient’s abdomen to perform the belly press test. The patient is directed to do an internal rotation by pressing the palm of his hand against his abdomen.
If the patient’s internal rotation was weaker on one side while it was stronger on the other, or if the internal rotation was absent when the patient was squeezed, the test was considered successful.
Treatment of Subscapularis Tendonitis
Conservative treatment is used for tendinopathy and subscapularis tendonitis. This often entails rest, changing one’s activities to stop the offending behavior, using cold packs, analgesics such as acetaminophen and NSAIDs, and physical therapy.
For most people, this means that their symptoms will go away. Instances of resistance can suggest that corticosteroid injections are necessary.
Subscapularis tendon tears are frequently misdiagnosed, thus a physician must have a high degree of suspicion. NSAIDs and physical therapy can be used to treat elderly people with a partial tear without surgery for a period of six to twelve weeks.
Pain relief and functional improvement may be achieved with a brief intra-articular injection. The patient ought to be sent to an orthopedist for a surgical examination if conservative treatment is not improving the situation.
A surgical examination is necessary for athletes, younger people, and anybody with a full-thickness tear. Either an open approach or an arthroscopic procedure is used for surgery. Pathology of the biceps often co-occurs and may need tenotomy or tenodesis.
Use the thumb method to massage the subscapularis muscle. First, feel the muscle contract; then, release the tension and begin rubbing. Be careful not to massage your nerves along with the muscle. If not, you might have discomfort for several days as you would have strained the nerves in your armpit rather than the muscle.
Exercise of Subscapularis Muscle
Stretching Exercise
Cross Body Arm Raise
A quick and efficient stretch for the subscapularis is the Cross Body Arm Raise.
Starting from a standing position with your feet shoulder-width apart, extend your arm forward on the side of the targeted muscle.
Grip your lifted arm slightly above the elbow with your opposite arm from behind, then gently draw it towards your body.
A comfortable stretch over the Subscapularis should feel good. Hold this posture for approximately 30 seconds, then release it gradually.
During this stretch, pay close attention to any feelings you have and get familiar with what feels comfortable. If you experience any unexpected pain or discomfort, stop right away.
If preferred, you may also execute this stretch while lying prone.
Cross Chest Stretch
Targeting the subscapularis muscle effectively involves stretching the chest muscles.
Start by either sitting up straight with your spine straight or standing with your feet shoulder-width apart.
Place the other hand next to the elbow and extend one arm across your chest.
When you feel a comfortable stretch in the front of your shoulder, slowly bring your arm closer to your body.
Hold this posture for 15 to 30 seconds, then release it and repeat on the other side.
Towel Stretch
An excellent and rather easy exercise for lengthening the Subscapularis muscle is the towel stretch.
Start by sitting or lying down on the ground, depending on how comfortable it is for you, and hold a towel firmly in both hands.
Bend the towel end to a 90-degree angle and wrap it over your forearm, just below your elbow.
Draw yourself as far away from it as you can by holding onto the other end of the towel. You should feel a steady, gentle stretch throughout your shoulder area.
The benefits of the stretch will become apparent to you right away. These benefits include improved range of motion, lessened localized pain and discomfort, and increased mobility. After maintaining this position for 15 to 30 seconds, switch to the other arm.
Internal rotation with abduction
To tie off one end of the resistance band right above your head, take a tall posture with your back to the stationary object.
Your hand reaches for another end.
With your arm out to the side, make a 90-degree angle movement.
To begin, rotate your arm downward against a band’s resistance until your palm is level with your hip.
Return to the starting position slowly, then repeat with the opposite hand.
Internal rotation stretch
Maintain a straight posture. For stretching, you’ll need a resistance band.
Tie one end of the resistance band around a stationary object and hold the other end in your hand.
Next, place your arm by your side with your elbow bent.
With your arm rotating across your abdomen, press it up against the resistance band.
Always keep your elbows close to your sides.
Hold it for 30 seconds when you start to feel stretched.
Proceed to perform on the opposite side.
Strengthening Exercises
Cable Standing Shoulder Internal Rotation
Positioned towards an elbow-height locking cable pulley, take a sideways position. As an alternative, apply a fitness band.
Using the arm nearest to the cable machine, grasp the cable handle. Keep your elbow tucked in at a 90-degree angle and locked against your side.
Pull the wire towards your body while internally rotating your shoulder until your forearm is crossed across your abdomen. Throughout the whole exercise, make sure to maintain a constant position with your elbow pushed against your side.
Once you’ve completed the required number of repetitions, go back to the beginning.
Repeat with your arms switched to the opposite.
Dumbbell Shoulder Internal Rotation
With a dumbbell in your right hand, lie on your right side on the floor. Keep your upper arm near your torso.
Hold the dumbbell straight above your elbow while bending your elbow 90 degrees. If needed, you can sag back a little to accommodate your whole range of motion.
Keeping the elbow at a 90-degree angle, lower the dumbbell towards the floor.
Your shoulder should feel stretched. For further support, you might grip your elbow with the hand on the other side.
Raise the dumbbell in the direction of your body while turning your shoulder inside out to make your forearm straight.
Continue till the desired number of times.
Turn over, then repeat with the other arm.